We present to your attention the material summarizing the long-term clinical experience with hyaluronic acid-based fillers and neuroprotein type A of the leading French specialist in the anatomy of injections, speaker of international congresses Philippe Questemon. This article was prepared based on the report at the INJECTION CONGRESS Academy by Dr. Mikhaylova. This knowledge will help you effectively and, no less importantly, safely perform procedures of contour plastic surgery and botulinotherapy.
Philippe Questemon, MD, maxillofacial surgeon, plastic surgeon of aesthetic head and neck surgery at St. George’s Aesthetic Clinic at University Hospital Center, member of the VISAGE scientific committee, head of the anatomy course in Nice, France.
The key to effective correction is a thorough knowledge of the anatomy of the areas where the cosmetologist intends to perform injections. Let’s start our review with the study of the anatomy of the upper part of the face. Then, in subsequent articles, we will consider the middle and lower third.
Forehead and eyebrow area
Beneath the skin in this area is fatty tissue, muscles with blood vessels, nerves and arteries. If the superficial fatty tissue is removed, the supraorbital muscle m. corrugator supercilia (the muscle that wrinkles the eyebrow) is located under the tendinous helmet; the main trunks of supratrochlearis and supraorbital (supraorbitalis) vascular-nervous bundles run in it. Muscle fibers of the frontal abdomen of m. occipitofrontalis
Beneath the skin in this area is fatty tissue, muscles with blood vessels, nerves and arteries. If the superficial fatty tissue is removed, the supraorbital muscle m. corrugator supercilia (the muscle that wrinkles the eyebrow) is located under the tendinous helmet; the main trunks of supratrochlearis and supraorbital (supraorbitalis) vascular-nervous bundles run in it. Muscle fibers of the frontal abdomen of m. occipitofrontalis
In the upper part of the eye socket is located the circular muscle of the eye (m. orbicularis oculi). Its medial part shows more dense tissue, which is often identified as a separate muscle that lowers the eyebrow (m. depressor supercilii). Other specialists, myself included, consider it to be part of the orbicularis oculi muscle. In the lateral part of the eye socket, the orbicularis oculi muscle is the depressor of the tail of the eyebrow. The muscle that wrinkles the eyebrow (m. corrugator supercilia) is deeper, very strong, and attaches directly to the bone.
Knowing the anatomy and the relationship of muscles to other structures is essential for safe and effective injections of neuroprotein type A. It also helps when modulating mimic muscle activity with hyaluronic acid-based fillers. For example, for greater contraction of the frontal muscles to raise the eyebrows, I inject deep, under the muscle, periosteally. Conversely, if I want to reduce the contraction of the facial muscles, I inject at the level of the subcutaneous fatty tissue – between the skin and the muscle.
(1) shows the effect of myomodulation after contouring in the superficial layer using a blunt-tipped cannula. The soft filler APRILINE® Normal (Suisselle, Switzerland) with a degree of reticulation of 9% was used. It is hyaluronic acid stabilized by the in one phase method according to the A. P. R. I. technology. P. R. I. TECHNOLOGY. This provides a 100% effectively crosslinked monophasic gel, as the crosslinking agent is bound to the hyaluronic acid molecule at both ends. The concentration of hyaluronic acid is 23 mg/mL. There is an excellent result of reduction of expression of expression of expression lines without botulinum therapy, only with the help of myomodeling technique. At the same time, the patient’s eyebrows did not become heavy or overhanging.

Patient before the procedure in static position (A), with active mimicry (C) and immediately after in static position (B) and during mimicry (D)
Next, let’s look at the structure of the upper part of the eye socket with the subcutaneous fatty tissue, the retro orbicularis oculi fat (ROOF). This is a very interesting area that can be seen by looking under the skin, m. frontalis and tendon helmet
Filling this area may be necessary in order to equalize the “sunken eye” effect. Inject very deeply, cupped, using a blunt-tipped cannula, because the injection trajectory crosses the supratrochlear (a. supratrochlearis) and supraorbital arteries (a. supraorbitalis). If you feel resistance during insertion, you should pull the cannula back and shift the direction slightly. This should be done very slowly and with extreme precision. The product of choice for filling this area is APRILINE® Normal with a degree of reticulation of 9%.

Insertion of APRILINE® Normal filler into the retro orbicularis oculi fat (ROOF) area using a blunt-tipped cannula.
Botulinum therapy of the upper third of the face
Consider from the anatomical point of view the introduction of neuroprotein type A in the upper third of the face. It was and remains the best means in the fight against facial wrinkles of the forehead area, glabella, “hound’s feet”. But, unfortunately, as with other invasive cosmetic procedures, there are risks of complications and undesirable effects if performed improperly. The most common of them in the upper third of the face – the lowering of the eyebrow or upper eyelid. Therefore, injections must be performed carefully to be sure that the lower part of the frontalis muscle, which is responsible for lifting the medial portion of the eyebrow, continues to function. By targeting type A neuroprotein to the brow depressor muscles, you will strengthen the activity of the m. frontalis, change the levator/depressor balance, and obtain a pharmacologic brow elevator effect.
A clinical case of complex correction is presented in. At the first stage, filling of the frontal area, supra- and suborbital fatty tissue (ROOF and SOOF) with hyaluronic acid-based fillers was performed. At the next stage, correction of the mimic muscles of the upper third of the face was performed using neuroprotein type A: frontal (m. frontalis); eyebrow lowering muscle (m. depressor supercilii); eyebrow wrinkling muscle (m. corrugator supercilia); lateral portion of the circular muscle of the eye (m. orbicularis oculis). Thus, using filler and neuroprotein, you will be able to correct the upper third of the face, restore architectonics and remove wrinkles.
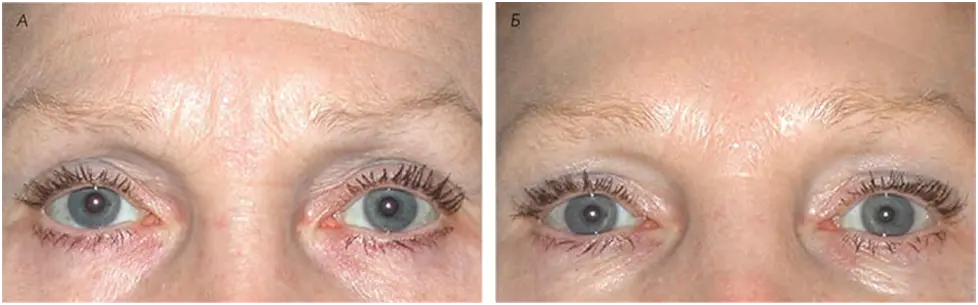
Patient before (A) and after (B) complex correction with hyaluronic acid and neuroprotein type A-based fillers.

Injections of neuroprotein type A in the lower eyelid area.
It is also possible to “open the eye” by injecting neuroprotein into the frontalis muscle and sometimes into the lower eyelid. In it can be seen how the injection is performed very superficially, in the projection of the preseptal part of the circular muscle of the eye.
When performing injection of neuroprotein type A in the glabella region, one should be very careful: if done at a height of 1 cm above the eyebrow, the result can be deplorable. It is necessary to stay at the same level (same line) as the eyebrow, so that the muscle that lowers the eyebrow (m. depressor supercilii) and the muscle that wrinkles the eyebrow (m. corrugator supercilia) can be safely corrected. If injected above the level of the eyebrow, the drug will enter the frontalis muscle and the desired result will not be obtained.
When neuroprotein type A enters or diffuses into the frontalis muscle, brow ptosis occurs. Even in the absence of expression lines, the result will be unsatisfactory. In addition, it is necessary to understand the difference between brow ptosis and eyelid ptosis, which is a consequence of ingestion of the drug into the muscle that raises the eyelid
Periorbital area
In the lower part of the eye socket is the SOOF – suborbicularis oculi fat. This fat pack is bordered by the ligament of the orbicularis oculi above, the zygomatic ligament below, the bone behind and the muscles in front. If the SOOF level is to be reached, it is necessary to cross all soft tissues with the cannula until it comes into contact with the bone. That is to say, make your way through the skin, zygomatic fat pack and muscle tissue. At this level you can see a thin fat layer, this is the SOOF – suborbicularis oculi fat. A cannula is used to work on this area, but since this is a fairly safe area, a needle can be used: by inserting it deeply and as close to the bone as possible, you can also get the desired results.
Care should be taken when using a needle, as the many blood vessels in this area can cause bleeding. The procedure using a needle is faster and less painful, but the risk of ecchymosis remains. The cannula insertion, on the other hand, is safer but also more painful. As for the lateral part of the suborbicularis oculi fat, it is definitely easier to work with a needle, as there are practically no large vessels in this area.
Shows the result of correction of the suborbicularis oculi fat area. The medial portion was filled with APRILINE® Normal with a reticulation rate of 9%, the lateral portion was filled with APRILINE® Forte medium density filler with a reticulation rate of 14%. This solved the problem of dark circles under the eyes as well as depression in the projection of the cheekbone area. A good result was obtained without any risks or consequences..

Patient before (A) and after suborbicularis oculi fat (SOOF) correction (B).
Temporal zone
Deeply injected bolus of stabilized hyaluronic acid.
The upper and lower part of the temporal zone differ significantly in terms of correction tactics. If its lower part is injected similarly to the upper part, a significantly larger amount of the drug will be required. Accordingly, to evenly distribute the filler, it is necessary to adapt the injection technique.
To fill the upper part of the temporal area, I use needle injections. It is necessary to pass through the skin, fat layer, injecting the filler under the deep temporal fascia. On the dissection preparation you can see the injected bolus, having previously “opened” the deep temporal fascia. It should be noted that the preparation remains in place, it does not migrate anywhere, because the muscle apparatus preventing hyaluronic acid from moving is concentrated in this area.
If you examine the lower temporal region, you can see a consistent arrangement of soft tissue, temporal fascia, tendon helmet and deep temporal fascia divided into two parts filled with fat pouches. You should not perform injections in this area with a needle because of the risk of embolization, as a large temporal artery passes here. Directly under the deep temporal fascia is located temporalis muscle. And it is in the lower temporal region, under the muscle, that we see the instrument easily pass into the deep space of the maxilla, so if stabilized hyaluronic acid is injected deep (cupped) in the lower temporal region, there is a risk of migration of the drug.
Thus, the upper part of the temporal region can be injected percutaneously with the needle without any problems. As for the lower part, a large amount of drug will be needed, and the risk of migration into the maxillary space must also be taken into account. For the upper part, I recommend using a needle and injecting a dense APRILINE® Forte filler with a reticulation rate of 14% deep down, while for the lower part of the temporal area it is preferable to use a blunt-tipped cannula and a soft APRILINE® Normal filler with a reticulation rate of 9%, distributing it at a superficial (subcutaneous) level. In this way, it will remain where it was injected without migrating into the underlying space.
The shows the result of temporal correction with two APRILINE® fillers of different densities

The instrument at the deep level passes easily through the inferior temporal region into the maxillary space.
Conclusion
We considered the algorithm of correction of aesthetic defects of the upper third of the face with fillers and neuroprotein type A based on facial anatomy. Knowledge of the topography and principles of facial tissue construction allows us to perform procedures safely and maximally effectively.