Minimally invasive rhinoplasty with neuroprotein type A and biodegradable fillers
The nose plays a crucial role in the overall aesthetics of the face. The authors of this article have developed an original minimally invasive approach to its correction, which you can use as an alternative to surgical rhinoplasty. The correction is performed according to certain rules, following which you can avoid most of the side effects and keep the results for a long time, earning the gratitude of your patients*.
Alessio Redaelli, professor at the University of Padua, Milan, Italy;
Pietro Limardo, otorhinolaryngologist, private practice, Lodi, Italy
The last decade has seen significant advances in cosmetic procedures: in particular, with the invention of materials of the highest safety profile, minimally invasive corrective procedures in the facial area have become possible.
The nose is extremely important not only as an odor-recognizing organ, but also as a key aesthetic element, because it is in the center of the face and visually linked to all adjacent structures, from the eyes to the mouth. Given the aesthetic importance of the nose, the possibilities of its aesthetic correction have been of interest to people since ancient times. The first evidence of the existence of surgical cosmetology appeared several millennia BC, particularly in the Far East and in Egypt in the era of the pharaohs. Correction of nose and ear deformities was popular at that time. Recall that a common punishment for unfaithful spouses was cutting off the nose. In the Middle Ages, the surgical school of the Branco family emerged. It was its representative Gaspare Tagliatozzi, the creator of the famous “Italian method” of nasal reconstruction after injuries and deformations. At the very beginning of the twentieth century, Jacques Joseph was named the father of modern surgical rhinoplasty. The external, or “open” method was first described by A. Reti in 1934, but this technique had not gained popularity until the early 1970’s, when it was first tried by W. Goodman. Interest in rhinoplasty as a technique, and the availability of a variety of invasive surgical techniques contributed to the development of the open method, which quickly gained recognition and popularity. To this day, however, there are differences of opinion regarding the preference for endonasal or external rhinoplasty [1].
The founder of modern medical rhinoplasty can probably be considered S. Brockert. It was he who first decided to correct the nasal profile with local injections of liquid paraffin – the first filler of the early twentieth century.
Currently, there is a trend towards less invasive treatment – that is, the desire to use the so-called minimally invasive techniques, including in rhinoplasty. With the advent of aesthetic cosmetology, it has become possible to correct many defects of the nasal profile, being limited to only small injections [2].
The method of minimally invasive medical rhinoplasty is based on two principles. The first is the control of the muscle activity of the nasal base, which is responsible for the movement and drooping of the tip, using botulinum neuroprotein type A (BNP); the second is the correction of nasal profile and age-related changes using biodegradable fillers. These principles, in turn, are based on precise, detailed rules described in the literature, which allow sufficiently qualified specialists in this field to learn how to achieve consistently positive results without significant side effects. The goal of both surgical and medical rhinoplasty is to achieve the desired aesthetic results without compromising the functionality of the nose. This is why it is very important for the surgeon and the cosmetic surgeon to know the methods thoroughly and to adhere to the principle of balance: the extent of the intervention is not as important as the harmony of the result.
Anatomy
Let us briefly review the anatomical structure of the nasal pyramid [3]. In the facial region we separate soft superficial and deep bony structures. The subcutaneous fatty tissue and muscular aponeurosis are much thinner in the nasal region than in other parts of the face.
The deep structures are represented by the fixed (nasal bone) and mobile parts (cartilage structure) (Fig. 1A). The cartilage of the nasal wings not only plays an important role in holding the nasal canal together, but is also extremely valuable for the aesthetics of the nasal tip. Just above the bony-cartilaginous layer are muscles united by a fibrous-aponeurotic complex called the SMAS (superficial musculoaponeurotic system). The muscles that raise, lower, contract and dilate the nostrils are important both functionally and aesthetically. The most important in terms of surgical and minimally invasive neuroprotein treatments are the muscles affecting the nasal tip, namely the muscle that lowers the septum of the nose and the muscle that raises the upper lip and wings of the nose (Fig. 1 B).
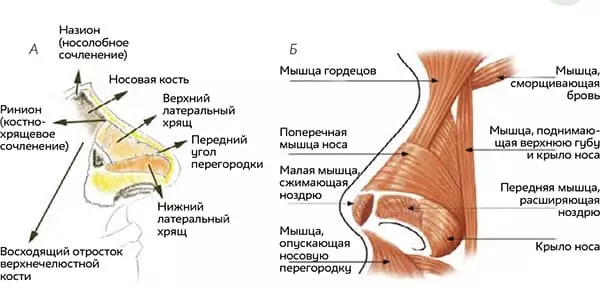
The blood supply is provided by the angular arteries arising from the intracranial vascular network in the upper corner, as well as the lateral and columellar arteries of the nose, arising from the superficial branches of the external carotid artery.
Motor innervation is provided by the facial nerve, and the sensory branches depart from the second branch of the trigeminal nerve and are represented by the external nasal, intraorbital, and nasolabial nerves. The surface of the nose is a skin rich in sebaceous glands, especially in the central-bottom part covering its cartilaginous part. The skin is tight in the medial part of the nose, less tight below in the tip area, and even looser in the root and frontal suture area.
Aesthetic Examination
Before undertaking any medical or surgical nasal correction, a thorough examination of the nasal area is necessary. This allows us to decide what to offer the patient and whether to offer anything [1, 3, 4].
The best option is to take five photographs of the patient in anteroposterior projection, at a 45° angle on the right and left, and in profile on the right and left sides. Next, the nasal pyramid should be examined in frontal view, and the symmetry of the wings and tip, the appearance of the choana, and the position of the nose relative to neighboring structures, particularly the eyes and mouth should be checked. In profile, the nasolabial angle, nasal dorsal angle, and nasolabial angle should be evaluated (Fig. 2). Cosmetic treatment is especially recommended if these angles are too small, particularly if the frontal angle is less than 120° and the nasolabial angle is less than 90°. The nasolabial angle is also important for minimally invasive surgical procedures, normally being about 35°; the nasolabial angle is about 125°. Based on these two angles, the projection of the nasal tip can be accurately determined.
An example of a patient with typical indications for medical rhinoplasty is shown in (Fig. 3). You can see that the nasolabial angle is too small (112°), and the situation can be significantly improved by injecting fillers into the nasal root area that increase the corresponding angle. The nasolabial angle is also too small (82°). Injections in the area of the nasal apex can also help to increase it.

FIG. 3 Patient with typical indications for medical rhinoplasty.

FIG. 2 Aesthetic examination.
It is also very important to observe the nasal tip in dynamics – when smiling or articulating during a conversation. This is best done at the very first visit, when the patient comes to the clinic and begins to talk about what he (she) needs. It is at this time, when the person is smiling and performing natural movements, that you can observe how the tip of the nose moves. If you specifically ask the patient to move their face or smile, the natural movement will be more difficult to see.
Surgical and minimally invasive methods
For a long time, surgical rhinoplasty has been considered one of the most challenging for the plastic surgeon, partly because of the dual function of the nose and its importance both aesthetically and functionally [2, 5].
Nowadays, surgeons are increasingly faced with the fact that patients want to simplify procedures – to minimize scars, reduce the volume of intervention and recovery period. Unlike other areas of surgical cosmetology, where minimally invasive alternatives are quite numerous, there are very few such options in the area of the nose.
There are two traditional approaches – open (external) and closed (endonasal) rhinoplasty – but there is no consensus on them either [2, 5, 6].
The endonasal technique emerged at a time when surgical techniques were formed and passed on from mentor to apprentice (Fig. 4A). When society was not as willing to accept surgical cosmetology as it is today, the focus was on making surgical scars invisible and creating the illusion of no surgery.
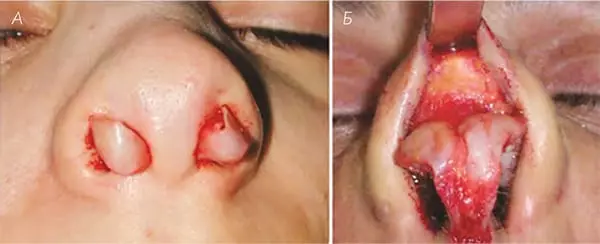
The main difference between the two methods is the degree of openness of the surgical site. With the open method, the entire osteochondral complex is visible in its natural state, without distortion, which allows for a more accurate assessment of the patient’s condition, diagnosis, and correction of the anatomy of the nose. This method allows you to directly see the lower nasal cartilages and the middle part of the septum. In addition, it has a number of technical advantages (Fig. 4 B): normal nasal anatomy can be restored, most often by correcting the location of the wing cartilage, as well as accurate placement and fixation of the cartilage plates (paired and forming the nasal tip). The main idea is the possibility to visualize the full picture of nasal anatomy, as endonasal methods allow to see most anatomical structures, but certain distortions still remain [4, 6].
The unconditional advantages of the endonasal method are that it allows you to work faster and requires less tissue excision [5], leaving less swelling and scarring [4]. Both methods can be operated using sedation or general anesthesia. Therefore, they are mostly considered suitable for outpatient procedures. In both cases a recovery period will be required.
Medical technique using neuroprotein and fillers
The medical technique of nasal profile correction [1] is based on the principle of correcting the overhanging nasal tip in the case of hypertonicity of the depressor muscles, in particular the septum descending muscle and the muscles raising the upper lip and wings of the nose. This is performed with a botulinum neuroprotein type A. In addition, we offer correction of the nasal profile with a biodegradable filler based on stabilized hyaluronic acid, which makes the result long-lasting – usually more than a year.
Correction of muscular hypertonicity with neuroprotein type A
Movement of the nasal tip in the direction of the maxillary bone is provided by the muscle lowering the nasal septum, and the muscle lifting the upper lip and nasal wings. It is not difficult to inject botulinum neuroprotein type A into them [1 – 9]. Injection into the muscle lowering the nasal septum can be performed on each side above the base of the columella (Fig. 5 A) and into the septum (Fig. 5 B). In this case, 2 to 4 units of 100-unit neuroprotein or 10 units of 500-unit neuroprotein are used.
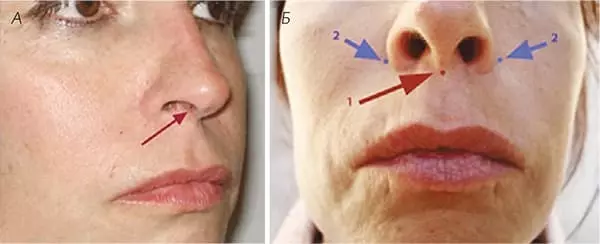
If there is hypertonicity of the upper lip and nasal wings muscle, clearly raising the sides of the nose and lowering the tip, 2 units of 100-unit neuroprotein or 10 units of 500-unit neuroprotein can be injected into the muscle, injecting on the sides of the nose as shown in (Fig. 5 B).
We will need to wait 7 to 15 days to evaluate the result. After 15 days, we always evaluate the result and supplement with a few more units of the drug if necessary.
It is important to be careful with the muscle that lifts the upper lip and the wings of the nose, as it is possible to accidentally lengthen the upper lip and thereby get ptosis. Young women with a gummy smile and a narrow (less than 1.5 cm) lip will have a lower risk than older patients (age 60 and older, with a wide lip). If there is less than 1.8 cm from the base of the nose to the top of the Cupid’s arch, this method is strictly contraindicated.
If there is hypertonicity of the upper lip and nasal wings muscle, clearly raising the sides of the nose and lowering the tip, 2 units of 100-unit neuroprotein or 10 units of 500-unit neuroprotein can be injected into the muscle, injecting on the sides of the nose as shown in (Fig. 5 B).
We will need to wait 7 to 15 days to evaluate the result. After 15 days, we always evaluate the result and supplement with a few more units of the drug if necessary.
It is important to be careful with the muscle that lifts the upper lip and the wings of the nose, as it is possible to accidentally lengthen the upper lip and thereby get ptosis. Young women with a gummy smile and a narrow (less than 1.5 cm) lip will have a lower risk than older patients (age 60 and older, with a wide lip). If there is less than 1.8 cm from the base of the nose to the top of the Cupid’s arch, this method is strictly contraindicated.
Correction of nasal profile and tip projection with biodegradable fillers based on stabilized hyaluronic acid
Safety is extremely important for optimal results. Therefore, we recommend the use of proven preparations with the highest safety profile.
We always start the procedure with local anesthesia by applying a topical preparation for at least 30 minutes.
The correction procedure itself usually starts from the root of the nose (Fig. 6A) and is performed by a linear retrograde injection on the bone, from the nasión to the interbrow area. The amount of preparation depends on the specific flaw to be corrected. The injection reveals the nasolabial angle; accordingly, it is primarily indicated in cases where this angle is less than normal – that is, less than 115°. If the nasolabial angle is also reduced (less than 90°), we then perform the injection at the base of the nose (Fig. 6 B), thereby opening this angle, which ideally should be more than 90°.
It is better not to try to do everything with one injection, but to go for the result step by step.

The last step focuses on the tip of the nose, which also often requires injection, especially if it is sagging. The injection is done in a thin subcutaneous layer, very slowly, to avoid ischemia of the skin above (Fig. 6 B). Here we use a fan technique, the correction is also best done in stages.
It is important to carefully check whether correction in two paired points is required (usually with a wider nose, especially in men) or if one central point (as is often the case in women) is sufficient. At the end of the procedure, we use an antiseptic to disinfect and apply post-procedure cream to reduce swelling, which is usually moderate. The patient can immediately return to his or her normal lifestyle.
The main indication for this procedure is any minor external nasal defects, in particular a downward pointing tip. The second important indication is a flat nose, which is often seen in dark-skinned patients and people of Asian descent. In these cases, it is also possible to narrow the wings of the nose.
Correction of postoperative problems
The method is also appropriate for correcting many postoperative deformities that are poorly amenable to other types of correction. In the case of excessive bone removal, especially in the area of the nasal root, with changes in the Shin lines and the appearance of a typical inverted V (Fig. 7 A), correction by injection of hyaluronic acid-based fillers allows immediate improvement. All this is uncomplicated and highly appreciated by patients [3] (Fig. 7 B).
In general, any small volume loss can be easily corrected with impressive results with low risk of side effects

FIG. 7 A – with the standard postoperative picture;
(B) – after elimination of the inverted V
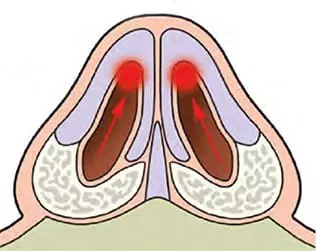
FIG. 8 Patient with typical indications for medical rhinoplasty.
Correction of functional disorders
Another indication for the use of stabilized hyaluronic acid refers to situations requiring correction from inside the nasal cavity, for example, in the case of sunken triangular septal cartilages during forced inhalation. In this case we use medium density stabilized hyaluronic acid (Fig. 8).
In all cases of atrophy of the nasal mucosa, as well as in chronic or atrophic rhinitis, we use only native (non-stabilized) hyaluronic acid for revitalization.
Conclusions
Nose profile defects, including a sagging tip, have been considered an indication for surgical correction in the last few years. With the advent of minimally invasive techniques, especially cosmetic correction, qualified cosmetologists have been able to correct a large number of minor imperfections. Although surgical correction often remains the benchmark, there are also worthy alternative methods that are well-received by these patients.
We see these methods as promising for the correction of functional impairments. In these cases, biointeractive and revitalizing hyaluronic acid effectively helps to moisturize and revitalize the nasal mucosa.
It is of utmost importance to properly qualify specialists who wish to apply these simple methods that promise excellent results. To always be on top of it and minimize the chance of side effects, you must strictly follow the rules detailed in the literature.





