Evaluation of the effective skin correction changes with plasma therapy – research results.
In recent years, patients of aesthetic medicine clinics prefer naturalness, so interest in plasma therapy has increased significantly, due to its high efficiency, availability and minimally invasiveness. The results of the study allow not only qualitative but also quantitative assessment of the results and benefits of the method.
Plasma therapy is widely used in the correction of involutional skin changes, treatment of acne and hair loss. It stimulates phagocytosis, has anti-inflammatory effects and the ability to accelerate regenerative processes due to the presence of platelet-derived growth factors in autologous plasma. This is particularly relevant for tissues with reduced healing potential, which is often evolutionarily altered skin. In addition, plasma has an immunomodulatory effect and improves tissue respiration [1, 2].
The essence of a method of plasma therapy consists in influence on tissues of numerous growth factors which are released from alpha-granules of blood platelets after injection into skin, stimulate metabolic processes, neocollagenogenesis and neoangiogenesis [3]. The (Fig. 1) shows the main growth factors. There are several brands of plasma therapy kits that have found use in medicine, particularly in cosmetology. Here are the most common ones:
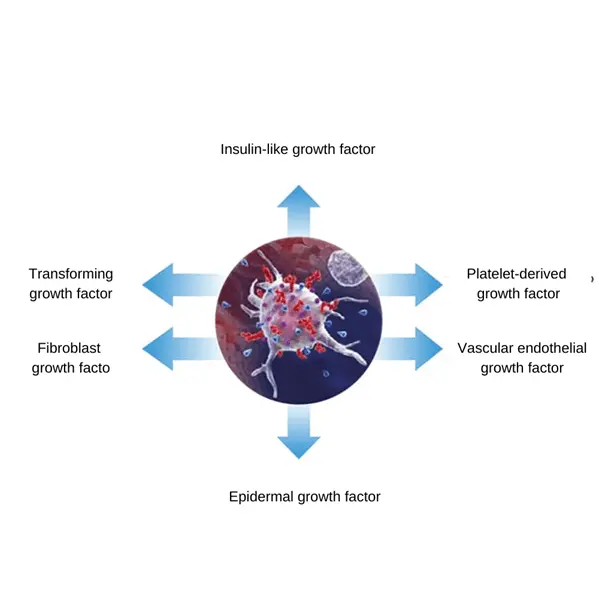
FIG. 1 Main platelet growth factors
Plasmolifting (LLC “Company “Plasmolifting”).
This technology has found wide application in correction of age-related skin changes and hair treatment, and has stable clinical results. The method makes it possible to obtain plasma with platelet content 33.8% higher than in whole blood. Heparin is used as an anticoagulant in the tubes, so ecchymosis can be a side effect of the procedure. Plasmolifting is performed as a course of 4 – 6 times with an interval between procedures of 7 days, which is not always convenient for patients living an active social life.
2. Regen ACR (Regen LAB SA, Switzerland).
This method is based not only on the introduction of autologous plasma, but also on fibrin autogel, rich in thrombin, which is obtained by a patented method, and without heating. The centrifuge retains up to 90% of live platelets, using sodium citrate as an anticoagulant and a special plasma activator. When injected into the skin, a three-dimensional fibrin network is formed in which platelets release growth factors over a long period of time. Several sets of tubes are available, so the method allows for differentiated selection of the procedure and correction protocol, depending on the initial state of the skin. The average course of treatment is 3 – 4 procedures with an interval of 3 – 4 weeks, which is convenient for patients. Sodium citrate is used as anticoagulant, which minimizes the risk of adverse reactions in the form of ecchymosis.
3. Endoret (BTI Biotechnology Institute S.L., Spain).
This method of PRP-therapy has proven to be highly effective and provides durable and predictable results in the correction of age-related changes, the treatment of inflammatory skin diseases, as well as hair restoration. After a course of therapy, a decrease in solar (photochemical) elastosis is noted, as well as, according to histological studies, there is a thickening of the epidermal and dermal layers of the skin, regardless of the age of the patients and the degree of photodamage. In addition, there is an increase in the number and more regular arrangement of collagen fibers [5].
Sodium citrate is used as anticoagulant, and a special proprietary activator (10% calcium chloride solution) is added to the obtained autologous plasma just before injection into the dermis, which promotes controlled and more complete degranulation of platelet alpha-granules. The result is PRGF (Plasma Rich in Growth Factors), which is injected intradermally and creates a 3D matrix in the skin, in which platelets continue to release growth factors for a long time, which explains the clinical effect. The course of treatment consists of 3 to 4 sessions at an interval of 3 to 4 weeks, side effects in the form of ecchymosis are rare, since sodium citrate, not heparin, is used as anticoagulant.
Below are the clinical results after a course of Endoret plasma therapy, which we use in our practice for more than three years.
Purpose of work
To study the influence of platelet-derived growth factors on the quality of involutionally altered skin, on the manifestations of photodamage: hyperpigmentation, skin microrelief as well as on the improvement of patients’ quality of life according to the adapted dermatological indices.
Materials and methods
The follow-up included 28 patients of the Center of Aesthetic Medicine “Astraja” aged 40-55 years (27 women and one man) with involutional changes and signs of skin photodamage such as hyperkeratosis, dyschromia, couperose. The patients were followed up for 6 months, the Endoret PRP-therapy protocol was performed, consisting of 4 procedures with an interval of 4 weeks.
Exclusion criteria for the study:
– pregnancy, breastfeeding period;
– Acute, including infectious diseases;
– Exacerbations of chronic somatic diseases;
– oncological diseases;
– mental disorders;
– autoimmune diseases;
– presence of thrombocytopenias and thrombocytopathies;
– intake of non-steroidal anti-inflammatory drugs, disaggregants.
To objectify the results of the study before and after 6 months, photodocumentation was performed using the LiveViz Quantificare 3D photo system, which allows to compare photos from the same angles and assess the dynamics of dyschromia reduction, improvement of skin microrelief.
Besides, all patients were asked to answer questions of adapted dermatological scales with high validity, which are widely used in researches – SUN (well-being-activity-mood) and DICH (dermatological life quality index, Dermatology Life Quality Index). The survey was conducted before the therapy and 6 months after.
The SUN Index, in its version adapted for cosmetology, is used for the rapid assessment of well-being, activity and mood by the patient himself. Changes in the data of this index reflect improvement in the quality of life of the interviewees, which indirectly indicates the effectiveness of the procedure.
Patients were asked to correlate their condition with a number of attributes on a multistep scale. The scale consists of numerical indices located between thirty pairs of words of opposite meaning, reflecting mobility, speed and pace of functions (activity), strength, health, fatigue (well-being), and characteristics of the emotional state (mood). The patient must select and mark the number that most accurately reflects his or her state at the time of the examination.
The Dermatological Quality of Life Index has high validity and is used to assess the quality of life of patients with dermatological diseases, in particular with pruritic dermatoses. Since involutional skin changes are not a nosological dermatological unit and are not accompanied by pronounced subjective sensations, such as skin itching, this index never has very high values in cosmetology and is used in a modified and adapted form for dynamic monitoring of changes in patients’ quality of life. The highest score obtained from patient responses corresponds to the lowest quality of life and is 30 points; the lowest score, to which the highest quality of life corresponds, is 0 points.
Methodology of the plasma therapy procedure
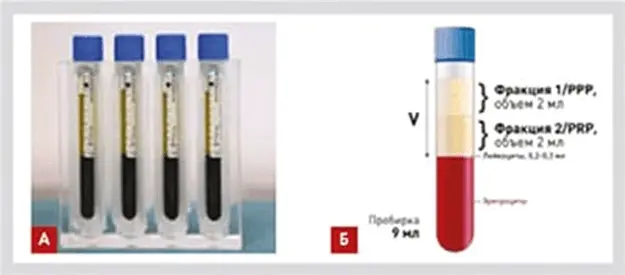
FIG. 2 Location of the PRP and PRP fractions in the test tube.
The PRP treatment procedure was performed after preliminary anesthesia application 4 times with an interval of 4 weeks. Blood was drawn from the cubital vein using a butterfly needle into two special extraction nine-milliliter tubes with anticoagulant (0.2 ml of 3.8% sodium citrate), venous blood in a total volume of 18 ml. These tubes were gently centrifuged using “floating beakers” technology at 580 g for 8 minutes at room temperature. The fractions obtained after centrifugation of whole autoblood were collected using a proprietary plasma transfer device and transferred to fractionated tubes: F1 fraction (PPP – Platelet Pure Plasma) and F2 fraction (PRP – Platelet Rich Plasma) (Figure 2). The PRP fraction is located on the border with dense fibrin clot, which separates plasma from blood form elements (erythrocytes and leukocytes) and contains 2.5 times more platelets with growth factors than in the original autoblood.
This fraction of 4 ml (2 ml from each tube) was taken into a syringe using long needles, and a proprietary BTI activator (10% calcium chloride in a dose of 50 µl per 1 ml of plasma) was added. The activator is necessary for growth factors to be released from platelets more completely and in a controlled manner. As a result, the resulting PRGF (Plasma Rich in Growth Factors) was injected intradermally into the patient using thin 31G needles in the volume of 0.1 ml per injection at a distance of 2 cm from each other. All patients tolerated the procedure of plasmotherapy well, side effects were observed in the form of transient hyperemia of the skin in the injection sites and sporadic ecchymosis, which resolved within 5 – 7 days.
Results
At follow-up examination of patients after 6 months from the beginning of the study, a high degree of patient satisfaction with the results of the therapy was noted (Table 1).
ТА BL. 1
Degree of patient satisfaction with the therapy performed
very satisfied 11 (39,3%)
satisfied 13 (46,4 %)
insignificant result 3 (10,7 %)
not satisfied 1 (3,6 %)
extremely dissatisfied 0
24 of 28 patients (85.7%) evaluated the clinical effect of the course of procedures as “satisfied” and “very satisfied,” which is a very high indicator for aesthetic procedures.
In addition, according to the results of the adapted dermatological scales, a pronounced improvement in the quality of life of patients was noted, which indirectly indicates the clinical effectiveness of the procedures performed.
The index “Feeling-activity-mood” increased both as a total and for each functional state of the body separately (Table 2).
TABLE. 2 Dynamics of changes in the SUN index scores over 6 months.
| index | before therapy | in 6 months |
| CAH total | 3,91 | 4,35 |
| Feelings | 3,91 | 4,33 |
| Аctivity | 3,93 | 4,34 |
| Mood | 3,90 | 4,38 |
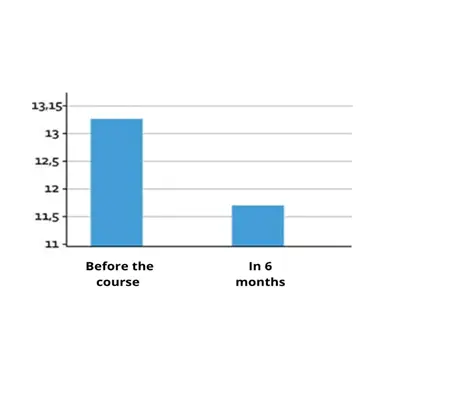
FIG. 3 Dynamics of changes in the dermatological index of the quality 11 of life.
Thus, the total index of the SUN index improved over six months by 11.25%, while the index of well-being increased by 10.74%, activity – by 10.43%, and mood – by 12.31%. These figures testify to the improvement of patients’ quality of life, especially their mood, which is a reflection of the efficiency of the performed therapy.
These changes in the dermatological index of quality of life correlate with the dynamics of improvement of the Feeling-Activity-Mood index. Over 6 months, this index decreased by 11.94%, which indicates an improvement in the quality of life of patients and indirectly indicates the clinical effectiveness of the therapy (Fig. 3).
Photodocumentation and comparison of three-dimensional images after six months showed improved skin quality, clearer facial contours (Fig. 4), reduced dyschromia (Fig. 5) and vascular pathology (Fig. 6).

FIG. 4 Results of 3D photo-documentation before and after 6 months (normal mode)
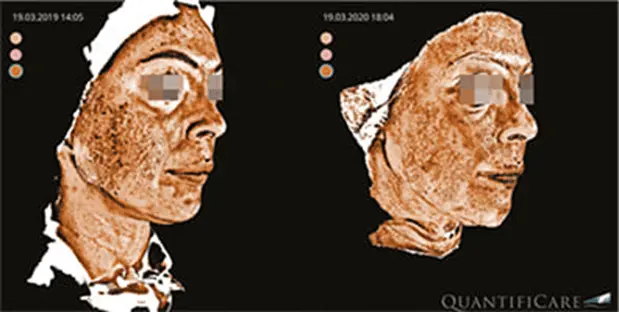
FIG. 5 Results of 3D photo-documentation before and after 6 months (pigmentation imaging mode).
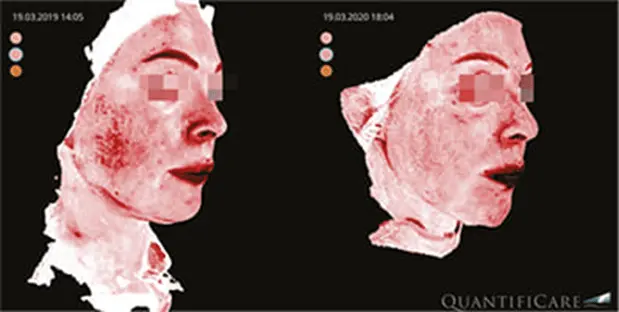
FIG. 6 Results of 3D photo-documentation before and after 6 months (vascular imaging mode).
Conclusion
PRP-therapy is a highly effective method of correction of involutional skin changes, allows to reduce the signs of skin photodamage, aligning its color and structure, so that the skin becomes more elastic and radiant. After a course of therapy improves complexion, reduces the number and severity of dyschromias and vascular abnormalities. The contours of the face become clearer, as therapy with autologous plasma stimulates fibroblasts, which under the influence of platelet-derived growth factors, increased synthesis of new collagen fibers, elastin, as well as its own hyaluronic acid. PRP-therapy has a pronounced anti-inflammatory effect, which allows using this method for treating acne disease, regulates the sebaceous glands and helps to reduce enlarged pores.
A very comfortable course of treatment, once every 3 – 4 weeks, allows patients not to interrupt their active social life.
PRP therapy complements many hardware methods, especially high-energy ones, allowing to achieve more pronounced results due to growth factors contained in the plasma, and to avoid post-traumatic hyperpigmentation by reducing the inflammation stage in the cascade of regenerative reactions.
Т. V. Stepanova, dermatologist, cosmetologist, physiotherapist, head of the physiotherapy department of the Center of Aesthetic Medicine.
Ж. Yusova M.D., Doctor of medical sciences, dermatologist, cosmetologist, physiotherapist, professor of the department cosmetology of the Central State Medical Academy of Postgraduate Education. Dermatologist, cosmetologist, physiotherapist, professor at the Department of Dermatology and Venereology and Cosmetology of the Central State Medical Academy.





